Adenocarcinoma is a type of cancer that develops in glandular cells. It can occur in various organs, including the lungs, pancreas, colon, and prostate. Treatment options may include surgery, radiation therapy, chemotherapy, targeted therapy, and immunotherapy. The specific treatment approach depends on the location and stage of the cancer.
Treating adenocarcinoma is crucial for managing the disease and improving survival outcomes. Surgery is often the primary treatment for localized tumors. Radiation therapy may be used to shrink tumors before or after surgery or to relieve symptoms in advanced stages of the disease. Chemotherapy involves the use of drugs to kill cancer cells throughout the body.
Targeted therapy and immunotherapy are newer treatment approaches that specifically target cancer cells or enhance the immune system’s ability to fight cancer, respectively. These therapies may be used in combination with traditional treatments to improve outcomes. The field of adenocarcinoma treatment is constantly evolving, with ongoing research aimed at developing more effective and personalized therapies.
Treatment for Adenocarcinoma
Adenocarcinoma, a type of cancer that originates in glandular cells, requires specialized treatment approaches. Here are eight key aspects to consider:
- Surgery: Removal of the tumor
- Radiation therapy: Uses high-energy radiation to kill cancer cells
- Chemotherapy: Employs drugs to destroy cancer cells
- Targeted therapy: Focuses on specific molecules involved in cancer growth
- Immunotherapy: Boosts the immune system to fight cancer
- Precision medicine: Tailors treatment based on individual tumor characteristics
- Palliative care: Manages symptoms and improves quality of life
- Clinical trials: Investigates new and innovative treatments
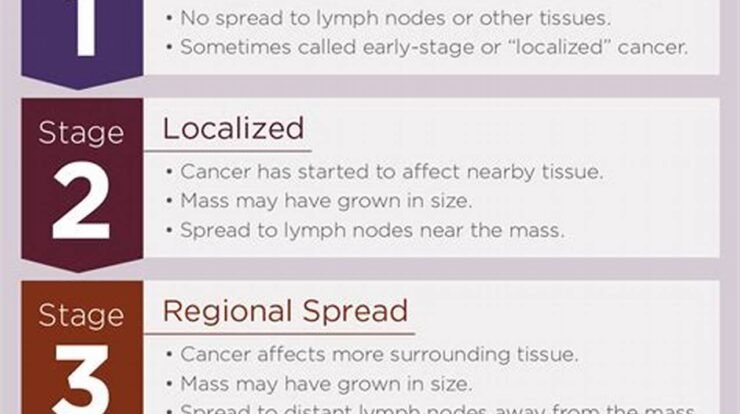
These aspects are interconnected and may be combined to provide comprehensive care. Surgery, for instance, can be followed by radiation therapy to enhance tumor control. Targeted therapy can be used alongside chemotherapy to improve treatment effectiveness. Precision medicine guides the selection of therapies based on the unique genetic makeup of the tumor. Clinical trials offer access to cutting-edge treatments and contribute to advancements in adenocarcinoma treatment.
Surgery
Surgery plays a critical role in the treatment of adenocarcinoma, often serving as the primary approach to eliminate the tumor. Its importance stems from several factors:
- Precise tumor removal: Surgery allows for the targeted removal of the cancerous tissue, minimizing damage to surrounding healthy cells.
- Control of tumor spread: By removing the primary tumor, surgery prevents the spread of cancer cells to other parts of the body.
- Improved treatment outcomes: Surgery can enhance the effectiveness of other treatments, such as radiation therapy and chemotherapy, by reducing tumor burden.
The type of surgical approach depends on the location and stage of the adenocarcinoma. For instance, in lung adenocarcinoma, surgery may involve removing a portion of the lung containing the tumor. In colon adenocarcinoma, surgery typically entails removing the affected part of the colon.
While surgery is often the preferred treatment for localized adenocarcinoma, it may not be suitable for all cases, especially if the cancer has spread or if the patient has other medical conditions. In such instances, alternative treatments, such as radiation therapy or targeted therapy, may be considered.
Radiation therapy
Radiation therapy plays a crucial role in the treatment of adenocarcinoma, particularly when combined with other modalities such as surgery and chemotherapy. Its effectiveness stems from several key factors:
- Targeted cell destruction: Radiation therapy specifically targets and destroys cancer cells by damaging their DNA, leading to cell death.
- Preservation of healthy tissue: Advanced radiation techniques, such as intensity-modulated radiation therapy (IMRT) and image-guided radiation therapy (IGRT), allow for precise targeting of the tumor while minimizing damage to surrounding healthy tissues.
- Enhanced treatment outcomes: Radiation therapy can improve the outcomes of surgery and chemotherapy by reducing tumor size, making it more susceptible to surgical removal or drug treatment.
In the context of adenocarcinoma, radiation therapy is commonly used in the following scenarios:
- Preoperative radiation therapy: Administered before surgery to shrink the tumor, making it easier to remove during surgery.
- Postoperative radiation therapy: Given after surgery to eliminate any remaining cancer cells and reduce the risk of recurrence.
- Palliative radiation therapy: Used in advanced stages of cancer to relieve symptoms such as pain and bleeding.
The use of radiation therapy in adenocarcinoma treatment requires careful planning and execution to ensure optimal outcomes while minimizing side effects. Collaboration between radiation oncologists, medical physicists, and other healthcare professionals is essential to deliver safe and effective radiation therapy.
Chemotherapy
Chemotherapy is a cornerstone of treatment for adenocarcinoma, a type of cancer that originates in glandular cells. Its significance lies in its ability to target and destroy cancer cells throughout the body, making it an essential component of comprehensive cancer care.
The effectiveness of chemotherapy in treating adenocarcinoma stems from its systemic nature. Unlike surgery or radiation therapy, which are localized treatments, chemotherapy delivers drugs intravenously or orally, allowing them to reach cancer cells wherever they may be in the body. This is particularly important for adenocarcinomas, which often spread beyond their initial location.
Chemotherapy drugs work by interfering with the growth and division of cancer cells. They target rapidly dividing cells, which is a characteristic of cancer cells. By damaging the DNA or other essential components of cancer cells, chemotherapy drugs induce cell death and prevent tumor growth.
The choice of chemotherapy drugs and the treatment regimen depends on the type and stage of adenocarcinoma, as well as the patient’s overall health. Chemotherapy can be used alone or in combination with other treatments, such as surgery, radiation therapy, or targeted therapy.
While chemotherapy is a powerful tool in the fight against adenocarcinoma, it is important to note that it can also cause side effects, such as nausea, vomiting, hair loss, and fatigue. These side effects vary depending on the type and dose of chemotherapy drugs used. Doctors carefully monitor patients during chemotherapy and provide supportive care to manage side effects.
Targeted therapy
Targeted therapy plays a crucial role in the treatment of adenocarcinoma, a type of cancer that arises from glandular cells. Its significance lies in its ability to specifically target and inhibit key molecules involved in the growth and survival of cancer cells.
Unlike traditional chemotherapy drugs, which often affect both cancer cells and healthy cells, targeted therapy drugs are designed to interfere with specific molecular pathways that drive cancer growth. By selectively targeting these pathways, targeted therapy can be more effective and have fewer side effects.
In the context of adenocarcinoma, targeted therapy drugs have shown promising results in treating various types of the disease. For example, drugs that target the epidermal growth factor receptor (EGFR) have been successful in treating lung adenocarcinoma, while drugs that target the HER2 protein have shown effectiveness in treating breast adenocarcinoma.
The development of targeted therapy has revolutionized the treatment of adenocarcinoma, providing new hope for patients with advanced or metastatic disease. Continued research in this field aims to identify new molecular targets and develop even more effective and personalized therapies.
In summary, targeted therapy has emerged as a critical component of the treatment landscape for adenocarcinoma, offering a more precise and effective approach to combating this type of cancer.
Immunotherapy
Immunotherapy has emerged as a groundbreaking approach to treating adenocarcinoma, a type of cancer that originates in glandular cells. Its significance lies in its ability to harness the power of the patient’s own immune system to fight cancer.
Unlike traditional cancer treatments such as surgery, radiation therapy, and chemotherapy, which directly target cancer cells, immunotherapy works by stimulating the immune system to recognize and eliminate cancer cells more effectively. This approach is particularly valuable for treating adenocarcinomas, which often develop resistance to conventional therapies.
In the context of adenocarcinoma, immunotherapy has shown promising results in treating various types of the disease. For example, immune checkpoint inhibitors have demonstrated efficacy in treating lung adenocarcinoma, while adoptive cell therapy has shown promise in treating bladder adenocarcinoma.
The development of immunotherapy has revolutionized the treatment landscape for adenocarcinoma, providing new hope for patients with advanced or metastatic disease. Continued research in this field aims to identify new immune targets and develop even more effective and personalized therapies.
In summary, immunotherapy has become an integral component of the treatment arsenal for adenocarcinoma, offering a unique and powerful approach to combating this type of cancer.
Precision Medicine
In the realm of treating adenocarcinoma, precision medicine has emerged as a transformative approach that revolutionizes treatment strategies by tailoring therapies to the unique molecular characteristics of each patient’s tumor.
-
Molecular Profiling:
Precision medicine utilizes advanced techniques like genomic sequencing and molecular profiling to identify specific genetic alterations or biomarkers within the tumor. This detailed molecular analysis helps uncover the tumor’s unique molecular fingerprint, guiding the selection of targeted therapies that are most likely to be effective.
-
Targeted Therapies:
Armed with the knowledge of the tumor’s molecular profile, physicians can select targeted therapies that specifically inhibit the growth and spread of cancer cells. These therapies are designed to interfere with key molecular pathways that drive tumor growth, offering more precise and effective treatment options.
-
Personalized Treatment Plans:
Precision medicine enables the development of personalized treatment plans tailored to each patient’s unique tumor characteristics. By matching the right therapy to the right patient, precision medicine aims to improve treatment outcomes, reduce side effects, and enhance the overall quality of life for patients with adenocarcinoma.
-
Improved Outcomes:
Clinical studies have demonstrated the remarkable benefits of precision medicine in treating adenocarcinoma. Patients who receive targeted therapies based on their tumor’s molecular profile have shown improved response rates, longer progression-free survival, and overall better outcomes compared to traditional treatment approaches.
In conclusion, precision medicine has revolutionized the treatment of adenocarcinoma by providing a deeper understanding of tumor biology and enabling the development of personalized, targeted therapies. This approach has significantly improved treatment outcomes, empowering physicians to tailor therapies to the unique molecular characteristics of each patient’s tumor.
Palliative care
Palliative care plays an integral role in the comprehensive treatment of adenocarcinoma, focusing on managing symptoms, improving quality of life, and providing holistic support to patients and their families.
-
Symptom Management:
Palliative care addresses the physical, psychological, and emotional symptoms associated with adenocarcinoma and its treatment. This includes managing pain, nausea, fatigue, anxiety, and depression, enabling patients to live more comfortably and with improved well-being.
-
Quality of Life Enhancement:
Beyond symptom management, palliative care emphasizes improving the overall quality of life for patients and their families. This involves addressing social, emotional, and spiritual needs, providing support systems, and promoting a sense of meaning and purpose.
-
Coordination of Care:
Palliative care teams collaborate with oncologists and other healthcare professionals to ensure a cohesive and patient-centered approach to treatment. They help coordinate care plans, facilitate communication, and provide ongoing support throughout the disease trajectory.
-
End-of-Life Care:
Palliative care is particularly important in the advanced stages of adenocarcinoma, providing compassionate and dignified end-of-life care. This includes managing pain and other symptoms, supporting emotional well-being, and assisting with decision-making.
In summary, palliative care is an essential component of the treatment for adenocarcinoma, offering a holistic approach that addresses the physical, psychological, and emotional needs of patients and their families. By managing symptoms, improving quality of life, and providing ongoing support, palliative care helps patients live more comfortably and with greater well-being throughout their journey with the disease.
Clinical trials
Clinical trials play a pivotal role in advancing the treatment landscape for adenocarcinoma. These trials investigate novel therapeutic approaches, evaluate their safety and efficacy, and contribute to the development of more effective and personalized treatments.
-
Exploring Novel Therapies:
Clinical trials provide a platform to test new drugs, drug combinations, and treatment modalities that have shown promise in preclinical studies. By evaluating these novel therapies in a controlled setting, researchers can determine their potential benefits and risks.
-
Evaluating Treatment Efficacy:
Clinical trials assess the effectiveness of new treatments by comparing them to standard therapies or placebos. This rigorous evaluation process helps determine whether the new treatment improves patient outcomes, such as survival rates, tumor shrinkage, or quality of life.
-
Identifying Predictive Biomarkers:
Clinical trials can also help identify predictive biomarkers that can guide treatment decisions. By analyzing tumor samples from patients in the trial, researchers can determine which patients are most likely to benefit from a particular treatment, enabling personalized treatment approaches.
-
Expanding Treatment Options:
The successful development of new treatments through clinical trials expands the therapeutic options available for patients with adenocarcinoma. This can lead to improved outcomes, reduced side effects, and increased survival rates.
In summary, clinical trials are essential for advancing the treatment of adenocarcinoma by investigating new and innovative therapies, evaluating their efficacy, identifying predictive biomarkers, and expanding treatment options. The insights gained from clinical trials contribute to the development of more effective and personalized treatments that improve patient outcomes and enhance their quality of life.
Frequently Asked Questions
This section addresses common questions and concerns regarding the treatment of adenocarcinoma, providing clear and informative answers.
Question 1: What are the different treatment options available for adenocarcinoma?
Adenocarcinoma treatment options vary depending on the location and stage of the cancer. Common treatment modalities include surgery, radiation therapy, chemotherapy, targeted therapy, immunotherapy, and palliative care. The specific treatment approach is determined by a multidisciplinary team of healthcare professionals.
Question 2: What is the role of surgery in adenocarcinoma treatment?
Surgery is often the primary treatment for localized adenocarcinoma. It involves removing the tumor and surrounding tissues to prevent the spread of cancer. The extent of surgery depends on the tumor’s location and size.
Question 3: How does radiation therapy work in treating adenocarcinoma?
Radiation therapy uses high-energy radiation to kill cancer cells. It can be used before or after surgery to shrink tumors or eliminate any remaining cancer cells. Radiation therapy is often combined with other treatments to improve outcomes.
Question 4: What are the side effects of chemotherapy for adenocarcinoma?
Chemotherapy drugs can cause a range of side effects, including nausea, vomiting, hair loss, fatigue, and low blood counts. The severity of side effects varies depending on the type and dose of chemotherapy drugs used. Doctors monitor patients during chemotherapy and provide supportive care to manage side effects.
Question 5: How does targeted therapy differ from traditional chemotherapy?
Targeted therapy drugs specifically target molecules involved in cancer cell growth and survival. Unlike traditional chemotherapy drugs, which affect both cancer cells and healthy cells, targeted therapy drugs are designed to minimize harm to healthy tissues. This can lead to fewer side effects and improved treatment outcomes.
Question 6: What is the importance of clinical trials in adenocarcinoma treatment?
Clinical trials play a crucial role in evaluating new and innovative treatments for adenocarcinoma. These trials investigate the safety and efficacy of new drugs and treatment approaches, contributing to the advancement of cancer care. Participation in clinical trials can provide patients with access to cutting-edge treatments and contribute to the development of improved therapies for future patients.
Remember, it is important to consult with a qualified healthcare professional for personalized advice regarding the treatment of adenocarcinoma.
Transition to the next article section:
For further information on adenocarcinoma treatment, please refer to the following resources:
- Resource 1
- Resource 2
- Resource 3
Tips for Managing Adenocarcinoma
Adenocarcinoma, a type of cancer that develops in glandular cells, requires specialized care and management strategies. Here are some essential tips to consider:
Tip 1: Seek Expert Medical Advice
Consult with experienced healthcare professionals who specialize in adenocarcinoma treatment. They can provide personalized guidance, recommend appropriate treatments, and monitor your progress.
Tip 2: Understand Your Diagnosis
Educate yourself about adenocarcinoma, its characteristics, and treatment options. Knowledge empowers you to make informed decisions and actively participate in your healthcare.
Tip 3: Explore Treatment Options
Discuss various treatment options with your healthcare team, including surgery, radiation therapy, chemotherapy, targeted therapy, and immunotherapy. Each treatment approach has its benefits and potential side effects.
Tip 4: Follow Treatment Recommendations
Adhere to the prescribed treatment plan and follow medical advice diligently. Regular check-ups and follow-up appointments are crucial for monitoring response and making necessary adjustments.
Tip 5: Manage Side Effects
Treatment for adenocarcinoma can cause side effects. Communicate any discomfort or symptoms to your healthcare team. They can provide medications or therapies to manage side effects and improve your quality of life.
Tip 6: Maintain a Healthy Lifestyle
Adopt a healthy lifestyle that includes a balanced diet, regular exercise, and stress management techniques. These measures can support your overall well-being and potentially enhance treatment outcomes.
Tip 7: Seek Emotional Support
Connect with family, friends, or support groups. Sharing your experiences and emotions can provide comfort and reduce feelings of isolation.
Remember, managing adenocarcinoma requires a collaborative effort between you and your healthcare team. By following these tips, you can navigate the treatment process more effectively and improve your overall well-being.
Transition to the article’s conclusion:
For further information and resources on adenocarcinoma management, please refer to the following:
- Resource 1
- Resource 2
- Resource 3
Conclusion
The exploration of treatment options for adenocarcinoma in this article highlights the advancements made in cancer care. From surgical interventions to targeted therapies and immunotherapy, the armamentarium against this type of cancer continues to expand.
Understanding the intricacies of adenocarcinoma, including its molecular characteristics, is crucial for developing personalized treatment plans. The role of precision medicine in tailoring therapies to individual patients holds great promise for improving outcomes. Furthermore, clinical trials remain essential for evaluating novel treatment approaches and expanding the therapeutic landscape.
As research continues and our knowledge deepens, we can anticipate further progress in the fight against adenocarcinoma. By fostering collaboration among healthcare professionals, researchers, and patients, we can work towards a future where this disease is effectively managed and ultimately conquered.
Youtube Video: